COVID-19 and Seasonal Allergies

An allergy (allergic rhinitis) that occurs in a particular season is more commonly known as hay fever . About 8 percent of Americans experience it.
Hay fever occurs when your immune system overreacts to an outdoor allergen, such as pollen. An allergen is something that triggers an allergic response. The most common allergens are pollens from wind-pollenated plants, such as trees, grasses, and weeds. The pollens from insect-pollinated plants are too heavy to remain airborne for long, and they’re less likely to trigger an allergic reaction.

Hay fever comes by its name from hay-cutting season. Historically, this activity occurred in the summer months, around the same time many people experienced symptoms.
Seasonal allergies are less common during the winter, but it’s possible to experience allergic rhinitis year-round. Different plants emit their respective pollens at different times of year. Depending on your allergy triggers and where you live, you may experience hay fever in more than one season. You may also react to indoor allergens, such as mold or pet dander.
Symptoms of seasonal allergies
Symptoms of seasonal allergies range from mild to severe. The most common include:
-sneezing
-runny or stuffy nose
-watery and itchy eyes
-itchy sinuses, throat, or ear canals
-ear congestion
-postnasal drainage
Less common symptoms include:
-headache
-shortness of breath
-wheezing
-coughing
Many people with hay fever also have asthma. If you have both hay fever and asthma, your seasonal allergens may trigger an asthma attack.

Causes of seasonal allergies
Hay fever happens when your immune system identifies an airborne substance that’s usually harmless as dangerous. It responds to that substance, or allergen, by releasing histamines and other chemicals into your bloodstream. Those chemicals produce the symptoms of an allergic reaction.
Common triggers of hay fever vary from one season to another.
Spring
Trees are responsible for most springtime seasonal allergies. Birch is one of the most common offenders in northern latitudes, where many people with hay fever react to its pollen. Other allergenic trees in North America include cedar, alder, horse chestnut, willow, and poplar.
Summer
Hay fever gets its name from hay-cutting season, which is traditionally in the summer months. But the real culprits of summertime seasonal allergies are grasses, such as ryegrass and timothy grass, as well as certain weeds.
Fall
Autumn is ragweed season. The genus name for ragweed is Ambrosia, and it includes more than 40 species worldwide. Most of them grow in temperate regions of North and South America. They’re invasive plants that are difficult to control. Their pollen is a very common allergen, and the symptoms of ragweed allergy can be especially severe.
Other plants that drop their pollen in the fall include nettles, mugworts, sorrels, fat hens, and plantains.
Winter
By winter, most outdoor allergens lie dormant. As a result, cold weather brings relief to many people with hay fever. But it also means that more folks are spending time indoors. If you’re prone to seasonal allergies, you may also react to indoor allergens, such as mold, pet dander,dust mites, or cockroaches.
Indoor allergens are often easier to remove from your environment than outdoor pollens. Here are a few tips for ridding your home of common allergens:
-Wash your bedding in very hot water at least once a week.
-Cover your bedding and pillows with allergen-proof covers.
-Get rid of carpets and upholstered furniture.
-Remove stuffed toys from your children’s bedrooms.
-Fix water leaks and clean up water damage that can help mold and pests flourish.
-Clean moldy surfaces and any places that mold may form, including humidifiers, swamp coolers, air conditioners, and refrigerators.
-Use a dehumidifier to reduce excess moisture.
Diagnosing seasonal allergies
Hay fever is usually easier to diagnose than other allergies. If you have allergic symptoms that only occur at certain times of the year, it’s a sign that you have seasonal allergic rhinitis. Your doctor may also check your ears, nose, and throat to make a diagnosis.
Allergy testing usually isn’t necessary. Your treatment for allergic rhinitis will likely be the same, no matter what type of allergen you react to.
Treating seasonal allergies
The best medicine for hay fever and year-round allergic rhinitis is avoidance of allergens that trigger symptoms for you. Medications are also available to treat symptoms of hay fever. Some people also try alternative treatments.
Avoidance
Take steps to avoid seasonal allergens. For instance, use an air conditioner with a HEPA filter to cool your home in summer, rather than ceiling fans. Check your local weather network for pollen forecasts, and try to stay indoors when pollen counts are high. At times of year when your hay fever is active:
-keep your windows shut
-limit your time outdoors
-consider wearing a dust mask when you’re outside, especially on windy days
It’s also important to avoid cigarette smoke, which can aggravate hay fever symptoms.
Medication
When you can’t avoid your allergens, other treatments are available, including:
over the counter decongestants and antihistamines, such as cetirizine (Zyrtec) and combination medications containing acetaminophen, diphenhydramine, and phenylephrine
prescription medications, such as steroid nasal sprays
In severe cases, your doctor may recommend allergy shots. They’re a type of immunotherapy that can help desensitize your immune system to allergens.
Some allergy medications may have unwanted side effects, such as drowsiness, dizziness, and confusion.
Alternative treatments
Few studies have been done on Alternative treatments for hay fever Some people believe the following alternative treatments may provide relief:
quercetin, a flavonoid that gives fruits and vegetables color
Lactobacillus asidophilus, the “friendly” bacteria found in yogurt
-spirulina, a type of blue-green algae
vitamin C, which has some antihistamine properties
More research is needed to learn if these alternative treatments are effective.
The takeaway
The symptoms of seasonal allergies can be uncomfortable. If you suspect you have seasonal allergies, talk to your doctor. They can help diagnose the cause of your symptoms and prescribe a treatment plan. They will likely encourage you to take steps to avoid your allergy triggers. They may also recommend over-the-counter or prescription medications.
What Are the Treatments for Allergic Rhinitis?

The first and best option is to avoid contact with substances that trigger your nasal allergies (allergens). When prevention is not enough, consider using over-the-counter or prescription medicines:
-Antihistamines are taken by mouth or as a nasal spray. They can relieve sneezing and itching in the nose and eyes. They also reduce a runny nose and, to a lesser extent, nasal stuffiness.
-Decongestants are taken by mouth or as a nasal spray or drops. They help shrink the lining of the nasal passages which relieves nasal stuffiness. These nose drops and sprays should be taken short-term.
-Nasal corticosteroids are used in nasal spray form. They reduce inflammation in the nose and block allergic reactions. They are the most effective medicine type for allergic rhinitis because they can reduce all symptoms, including nasal congestion. Nasal corticosteroids have few side effects.
-Leukotriene receptor antagonists block the action of important chemical messengers other than histamine that are involved in allergic reactions.
-Cromolyn sodium is a nasal spray that blocks the release of chemicals that cause allergy symptoms, including histamine and leukotrienes. This medicine has few side effects, but you must take it four times a day.
Nasal allergy symptoms may disappear completely when the allergen is removed or after the allergy is treated. Talk to your pharmacist and health care provider about what is best for you.
Many people with allergies do not get complete relief from medications. They may be candidates for immunotherapy. Immunotherapy is a long term treatment that can help prevent or reduce the severity of allergic reactions and change the course of allergic disease by modifying the body’s immune response to allergens.
How Can I Prevent Allergic Rhinitis?
The first and best option is to avoid contact with allergens. Other prevention tips are:
-Don’t touch or rub your nose.
-Wash your hands often with soap and water.
-Use a vacuum with a certified asthma & allergy friendly filter to reduce allergen exposure while vacuuming.
-Wash your bed linens and pillowcases in hot water and detergent to reduce allergens.
-Use dust-mite proof covers for pillows, comforters, duvets, mattresses and box springs.
-Keep pets out of the bedroom to reduce pet dander allergen in your bedding.
-Wear sunglasses and a wide-brimmed hat to reduce pollen getting into your eyes.
-Keep windows closed during high pollen and mold seasons. Use the air conditioner in your car and home

COVID-19 is a contagious respiratory illness caused by infection with a new coronavirus (called SARS-CoV-2, the virus that causes COVID-19). Seasonal allergies triggered by airborne pollen can lead to seasonal allergic rhinitis, which affects the nose and sinuses, and seasonal allergic conjunctivitis, which affects the eyes.
COVID-19 and seasonal allergies share many symptoms, but there are some key differences between the two. For example, COVID-19 can cause fever, which is not a common symptom of seasonal allergies. The image below compares symptoms caused by allergies and COVID-19.
Because some of the symptoms of COVID-19 and seasonal allergies are similar, it may be difficult to tell the difference between them, and you may need to get a test to confirm your diagnosis.
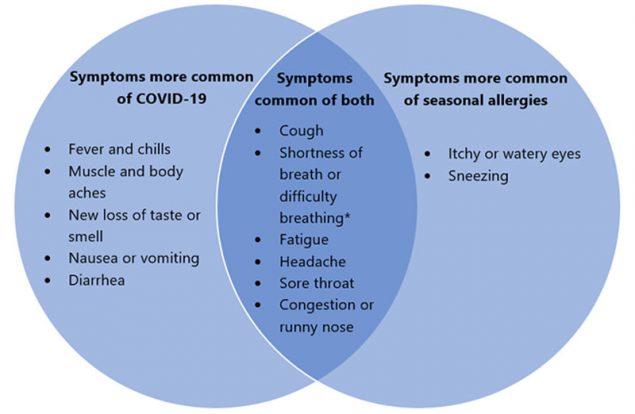
*Seasonal allergies do not usually cause shortness of breath or difficulty breathing, unless a person has a respiratory condition such as asthma that can be triggered by exposure to pollen.
This is not a complete list of all possible symptoms of COVID-19 or seasonal allergies. Symptoms vary from person to person and range from mild to severe. You can have symptoms of both COVID-19 and seasonal allergies at the same time.
There is not enough scientific information at this time to know whether having seasonal allergies puts you at higher risk of contracting COVID-19 or having more severe symptoms if you do contract COVID-19. We do know that older adults and people who have severe underlying medical conditions like obesity, diabetes, or heart or lung disease are at higher risk for developing more serious complications when they have COVID-19. Get more information on people at high risk for severe covid-19.
wearing masks to slow the spread of COVID-19. Everyone should wear a mask covering unless they are under 2 years of age, have breathing problems, or are unconscious or incapacitated and would need assistance removing a mask. Masks also offer some protection against seasonal allergies because they can prevent some larger particles from being inhaled. However, if you have seasonal allergies, masks should not be your only protection against pollen exposure because smaller particles can still get through the covering and be inhaled.
Wash your masks after each use, particularly if you suffer from seasonal allergies, because the covering may carry particles such as pollen. See information on how to wash masks.
The best way to protect yourself against seasonal allergies is to reduce your exposure to pollen. During high pollen days:
-Limit your time outdoors and seek indoor spaces with clean air.
-Create a cleaner air space at home to protect yourself from outdoor air irritants during the COVID-19 pandemic. Use a portable air cleaner in one or more rooms. Portable air cleaners work best when run continuously with doors and windows closed.Do it yourself box fan filtration units are a low-cost filtration alternative, but they should never be left unattended.
-Keep your cleaner air space a comfortable temperature by using air conditioners, heat pumps, fans, and window shades.
-If you have a forced air system in your home, consult a qualified heating, ventilation, and air conditioning (HVAC) professional about different filters (HEPA or MERV-13 or higher) and settings (“Recirculate” and “On” rather than “Auto”) that can be used to reduce indoor air irritants.
-If outdoors, avoid activities that stir up pollen, such as mowing lawns or raking leaves. When you return indoors, take a shower and change your clothes.

Prepared:
Neshat Khosravi – Microbiologist
Refrence:
https://www.healthline.com-https://www.cdc.gov






Recent Comments